How ASKP3 is Leading the Way on Ketamine Therapy Policy and How You Can Take Action in Your State
INTRODUCTION FOR FIRST-TIME ADVOCATES
What is Advocacy and Why You Should Care
If you’re a clinician, you’re already an advocate. You advocate every day for your patients, your staff, and your standards of care. Advocacy in the policy arena is simply an extension of that work: it’s how we speak up to shape the rules that govern how we practice.
Advocacy means showing up — not shouting. It means sending a letter, joining a meeting, signing onto a coalition, or sharing your story with decision-makers. It can take as little as ten minutes, but the impact is lasting.
Why it Matters Now
Ketamine therapy is saving lives, especially for patients with treatment-resistant depression, PTSD, and suicidality. However, many state rules were written for surgical anesthesia, not mental health care. That mismatch puts patients and providers at risk.
Without a tailored regulatory framework, clinicians are left to guess whether they’re compliant. Worse, bad actors exploiting loopholes create headlines that threaten access for everyone.
Your voice, as a licensed medical professional providing safe, evidence-based care, is the most credible force for change.
ASKP3 is here to help! We’ve led successful advocacy efforts in Texas and are now building a national coalition of clinicians, therapists, and advocates who want to do the same in their states.
HOW KETAMINE IS REGULATED
The State/Federal Landscape
Ketamine is a Schedule III controlled substance regulated under the federal Controlled Substances Act by the Drug Enforcement Administration (DEA). In 2019, the Food and Drug Administration (FDA) approved the use of intranasal esketamine to treat treatment-resistent depression under the brand name Spravato. All other modalities of ketamine treatment, including intravaneous, intramuscular, and oral, are considered “off-label” by federal guidance when used in a mental health setting.
State Legislators and Regulators largely determine key issues, such as:
- Who can prescribe and administer ketamine?
- What safety protocols are required?
- Does ketamine for mental health fall under anesthesia rules?
- Are clinics required to register or meet facility standards?
Because this treatment modality is relatively new, there is not yet a consensus regarding best-practices and that, together with the fact that the laws vary on a state-by-state basis, can lead to confusion, challenges in terms of implementing compliant programs, and inconsistent access for patients. That’s where state-level advocacy comes in.
Who Regulates the Prescribing and Administration of Ketamine in Your State?
Regulation typically falls to a combination of:
- State Medical Boards — oversee physician practice and delegation
- State Nursing Boards — oversee nursing practice and standards of care
- State Boards of Pharmacy — govern controlled substances and dispensing
- Departments of Health or Consumer Protection — may license clinics or enforce public health policy
ASKP3 has compiled a 50-state database of these regulatory agencies, (as of October 2025) complete with:
- The state-specific board(s) that oversee ketamine use;
- What their scope of authority includes; and
- Direct search links to each agency website.
Access the State-by-State Ketamine Regulatory Guide (Google Sheet)
THE ASKP3 ADVOCACY MODEL
How We Changed the Conversation in Texas — And How You Can Do the Same
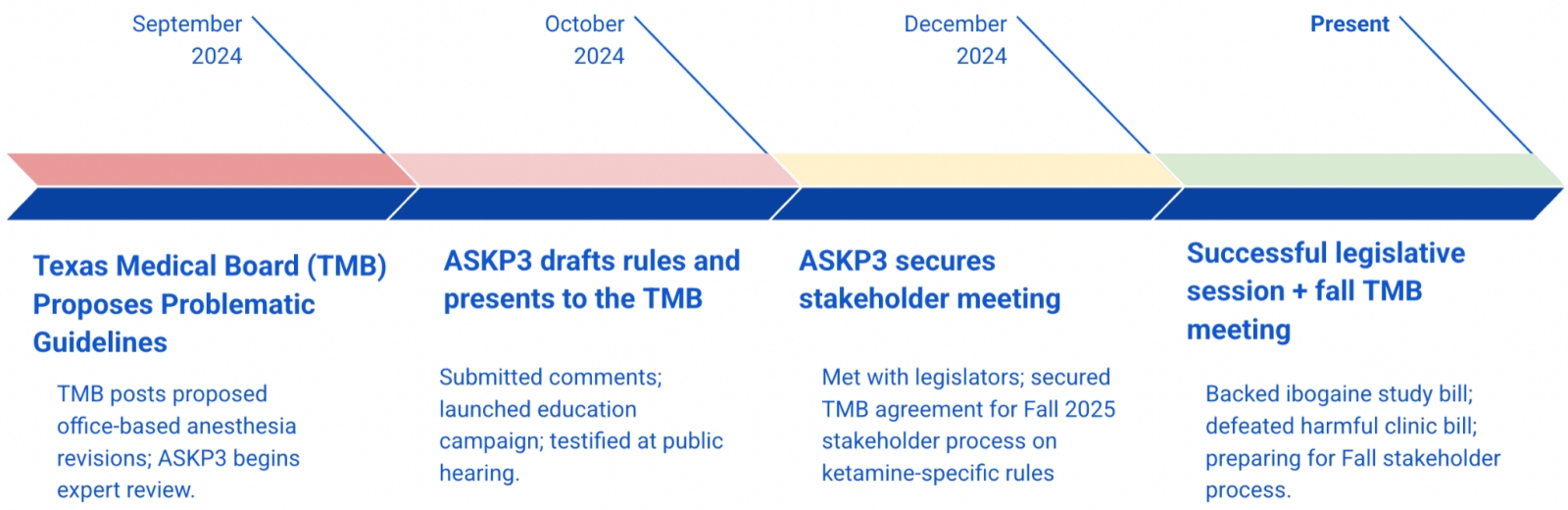
In late 2024, the Texas Medical Board (TMB) proposed significant changes to its regulations, including those related to Office-Based Anesthesia (OBA), which was relevant to ASKP3, because the administration of ketamine for mental health, even in very small doses, arguably triggered to OBA rules. ASKP3 offered comments to those rules in an effort to promote our vision that ketamine mental health therapy should be excluded from OBA compliance regulations. Because of unrelated issues, the TMB did not accept at that time, but responded favorably to our recommendations and suggested further discussion on the issue after the then current legislative session.
ASKP3 stepped in, not just to defend access — but to lead with a solution.
The Texas Playbook: A Case Study
September 2024
In Texas, the Medical Board (TMB) oversees the Office-Based Anesthesia (OBA) program, which was designed to regulate surgical settings and procedures performed outside of hospitals, ASCs, and other facility settings, where patients are placed under deep sedation or anesthesia. Clinics operating in Texas that provide subanesthetic ketamine therapy for mental health are not performing surgery, not putting patients “under,” and not engaging in procedures with comparable risks. Despite this, the OBA rules have been applied to our members, creating costly and unnecessary burdens. Under the rules, we are required to meet hospital-grade staffing, training, and equipment standards, which are appropriate for surgery but not for a safe, controlled, low-dose ketamine session. We do not believe OBA should capture our practice for these reasons.
When the new rules were proposed in 2025, in an effort to clarify the language, the TMB offered a legal framework that could arguably have made it even harder to argue that subanesthetic doses of ketamine treatments fall outside the bounds of the OBA rules. The rules also added ASA terminology updates, included nitrous oxide and oxygen in Level I, expanded acceptable certifications (adding PeRLS), and reorganized equipment and monitoring requirements by anesthesia level. While intended as clarifications, these changes increase complexity and created confusion among providers.
In response, we convened our expert faculty and engaged a broad cross-section of members to draft formal comments and propose a new section of the rules tailored explicitly to ketamine therapy for psychiatric indications in mental health settings. This proposed framework recognizes the unique safety profile of subanesthetic ketamine, preserves physician leadership, ensures appropriate advanced practitioner support, and maintains robust patient safeguards without imposing surgical-level requirements that add cost and reduce access without improving outcomes.
October 2024
ASKP3 submitted formal written comments to the Texas Medical Board detailing our concerns with the proposed OBA revisions and their impact on mental health ketamine clinics. At the same time, we launched a targeted education campaign to policymakers and agency staff, providing clear, fact-based materials to explain why these rules are ill-suited for subanesthetic ketamine therapy. Our President and members of the Board testified at the public hearing, sharing clinical expertise and patient care perspectives that highlighted the need for a dedicated regulatory framework.
- To read our full talking points and answers to common questions, click here.
- To review our complete written comments, click here.
December 2024
ASKP3 engaged in a series of one-on-one meetings with key legislators and agency leadership to press the case for a fair, medically appropriate regulatory approach to ketamine therapy in mental health settings. The Texas Medical Board initially rejected our proposed solutions, stating they were too substantive to address through a simple regulatory amendment. In response, ASKP3 urged the Board to initiate a formal stakeholder process to explore ketamine-specific rules that reflect clinical realities while maintaining patient safety. The TMB agreed, committing to convene a stakeholder process in early fall 2025 to thoroughly evaluate and consider this important policy shift.

Governor Greg Abbott signs Senate Bill 2308 to fund clinical studies on ibogaine.
Spring/Summer 2025
During the legislative session, ASKP3 actively engaged at the Capitol to protect access to innovative mental health treatments. We helped secure passage of legislation to fund clinical studies on ibogaine for veterans and individuals with PTSD, marking a significant step forward in psychedelic research and treatment options. At the same time, we successfully defeated harmful proposals that would have imposed unnecessary and burdensome regulations on Texas ketamine clinics. Looking ahead, ASKP3 continues to work closely with the Texas Medical Board in preparation for the formal stakeholder process in the fall of 2025, ensuring our members’ voices and patient care priorities remain at the forefront of the conversation.
What Made it Work
Lead With Solutions
ASKP3’s aim was to propose an alternative to opposition to the rules with a physician-led, clinic-based regulatory framework with tailored safety protocols for subanesthetic ketamine.
Use Multiple Channels
We submitted written comments, testified publicly, held in-person meetings, and launched an educational campaign to legislators and the public.
Build Credibility
We brought data. We brought doctors. We brought patients and veterans. And we clarified the clinical distinction between anesthesia and psychotropic therapy.
Broaden the Tent
We worked with the Texas Medical Association, veteran advocates, mental health nonprofits, and public health experts to build a unified voice.
What You Can Replicate in Your State
ASKP3 is helping members follow this model across the country. Here’s how you can adapt it:
Tactic | What It Looks Like in Your State |
Identify the Policy Driver | Use our state lawmaker and regulatory database to find who oversees ketamine in your state |
Monitor Rules | Check if ketamine is mentioned in anesthesia or other state-specific statutes or regulations (like OBA in Texas) |
Submit Comments | Use ASKP3’s templates for public comment letters and testimony |
Schedule Meetings | Meet with elected officials, regulators, and their staff to educate them on ketamine therapy |
Build a Coalition | Connect with physician/nursing associations, psychiatric societies, veteran groups, and patient advocacy networks |
Educate with Evidence | Use our fact sheets and talking points to clarify the difference between anesthesia and subanesthetic mental health care |
ASKP3 and our member network can help along the way. Our expert staff and network of advocates are ready to serve.
“We weren’t just heard — we helped shape the future of ketamine regulation.”
– Dr. Sandhya Prashad, ASKP3 Board Member
YOUR ADVOCACY CAMPAIGN: A STEP-BY-STEP ROADMAP
Phase 1: Understand the Landscape
- Find and contact your local lawmaker (click here). Ask them for a virtual or in-person meeting to discuss your practice. Are they on relevant committees to be helpful? Are they willing to advocate for you?
- Identify your state’s regulatory agency (click here). A great exercise to understand the rules, the players, and the decision makers who set policy and influence the legislature.
- Review how your state defines or regulates sedation, anesthesia, or dissociative drugs — and whether ketamine is included.
- Confirm your clinic’s current legal positioning (consult if needed).
Phase 2: Organize Your Toolkit
- Contact ASKP3 for the latest templates.
- Recruit 2–3 local allies: a therapist, a psychiatrist, a veteran, a patient.
- Build a simple “one-pager” on your clinic’s outcomes and safety protocols.
Phase 3: Take Action
- Submit public comments using ASKP3 templates.
- Request meetings with your medical board and local legislators.
- Speak at public hearings or offer written testimony.
- Share your clinic’s story with one reporter or local media outlet.
Phase 4: Stay Involved
- Track outcomes and share progress with ASKP3.
- Help other members in your state do the same.
- Volunteer to be part of a statewide coalition or working group.

